Pharmacogenomics, which looks at how a person’s genes affect their response to medicine, is often called one of the most exciting areas of modern medicine. Instead of giving everyone the same drug at the same dose and hoping it works, doctors can use genetic testing to choose the best medication for a patient. This could mean fewer side effects, more effective treatment, and less wasted money on drugs that do not work.1 When the Human Genome Project finished in 2003, scientists thought this type of medicine would quickly become common. Almost twenty years later, pharmacogenomics is finally showing real results in hospitals and clinics. But there is a big problem: not everyone has the same chance to benefit from these new advances. Genetic testing is expensive, it is not always covered by insurance, and it is usually found in large hospitals in big cities. People in rural areas or with low income may never be offered it at all. That creates a fairness issue, because healthcare advances should be available to all patients, not just the wealthy.2 It seems that pharmacogenomics really does have great potential, but it can only be considered ethical if access is made more fair. Looking at the science, the different viewpoints, and the requirements for fairness, it becomes clear that the future of pharmacogenomics depends on whether society chooses to share its benefits equally.
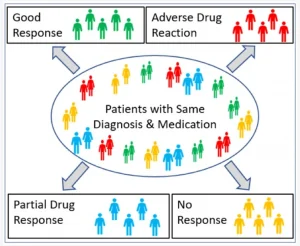
There are many clear examples of how pharmacogenomics helps patients. Warfarin, a common blood thinner, has been hard for doctors to prescribe because people react very differently to it. Too much can cause bleeding, and too little can fail to prevent clots. It turns out that differences in the CYP2C9 and VKORC1 genes explain a lot of this variation. Patients with certain versions of these genes break the drug down slowly, so they need lower doses to stay safe. Without this information, doctors often have to spend weeks adjusting the dose through trial and error. Testing makes it possible to start patients at the right dose and avoid serious side effects.3 Another case is abacavir, a drug used to treat HIV. Around 5–8 percent of patients used to suffer from a dangerous allergic reaction to abacavir. Researchers later discovered that people with the HLA-B*57:01 gene variant were most at risk. Now, most doctors test for this gene before prescribing abacavir, and the allergic reaction has almost disappeared in clinical practice.4 Cancer treatment is another area where pharmacogenomics makes a huge difference. For example, women with breast cancer who test positive for the HER2 marker can benefit from trastuzumab (Herceptin), while women without it do not. Using this test helps doctors give the right treatment to the right patient. In leukemia, patients with certain TPMT gene variants metabolize chemotherapy drugs differently, and testing prevents toxic overdoses. The benefits go beyond single drugs. Adverse drug reactions cause over 700,000 ER visits and more than 100,000 deaths every year in the U.S. alone.5 A study in 2024 showed that patients who received pharmacogenomic-guided care had 39 percent fewer hospitalizations and ER visits compared to those who did not.6 These results show that pharmacogenomics is not just an exciting theory. It is already improving safety and saving money. From a Catholic Intellectual Tradition (CIT) perspective, these medical successes reflect humanity’s creative participation in God’s design through science. The Church recognizes scientific progress as good when it serves life and human dignity. However, the CIT also emphasizes the moral virtue of prudence, the ability to act wisely by considering consequences and justice. If pharmacogenomics improves lives but is only available to the wealthy, it risks violating the moral duty to serve the common good. As the Pontifical Academy for Life (2019) reminds us, technological innovation must never outpace ethical reflection, especially when it involves human health and equality.7

Doctors and researchers who support pharmacogenomics often say it is a moral duty to use it. If we know a genetic test can prevent harm or save lives, it feels wrong not to use it. They also argue that costs will go down as testing becomes more common, just like other technologies in medicine. They believe that once it is fully implemented, everyone will benefit. Supporters also point out that it can save the healthcare system money overall by avoiding wasted prescriptions and hospital stays.8 Patients see things differently. For many, the idea of medicine designed for them personally is exciting. But a lot of patients are disappointed when they find out they cannot get the test where they live, or their insurance will not cover it. Imagine two patients: one in Boston at a major hospital gets pharmacogenomic testing as part of normal care, while another in rural Texas may not even be told it exists. The second patient might end up with side effects or ineffective treatment simply because of where they live. That feels unfair and also reduces trust in the healthcare system. From the Catholic view, this difference in access challenges the virtue of justice, which is central to the CIT. Justice calls for fairness, equality, and the protection of vulnerable people. In medicine, justice means that all people deserve access to life-saving tools, not just those who live in certain areas or can afford certain tests. The Church’s emphasis on the common good also reminds us that scientific knowledge carries a shared responsibility. Pharmacogenomics should not serve profit or privilege but the well-being of all. Critics focus more directly on equity. Salari and Larijani (2017) warn that if access to pharmacogenomics stays uneven, it will make existing health inequalities worse.9 Magavern (2023) also notes that within health systems, richer and urban patients tend to get new technologies first, while poorer and rural patients are left waiting.10 Globally, the contrast is even bigger. Wealthy countries are investing heavily in pharmacogenomic infrastructure, while low- and middle-income countries often struggle to afford basic medicines, let alone advanced genetic testing. This means pharmacogenomics could become yet another example of the gap between rich and poor countries. Privacy and consent issues make the debate even more complicated. Genetic data is sensitive and permanent. Patients may not fully understand that their results could affect not just them, but also family members who share their genes. Once the data is collected, it may be stored for decades and possibly used for other research. Yunta (2022) explains that laws like the U.S. Genetic Information Nondiscrimination Act (GINA) protect people in some cases, but there are still gaps.11 For example, life insurance and long-term care are not fully covered. CIT values like respect for human dignity and solidarity apply directly here. The Church teaches that every person, regardless of background or genetics, deserves to be treated with respect and the protection of privacy. Solidarity means recognizing our shared responsibility to one another, especially the most vulnerable. Therefore, genetic testing must be used in ways that protect people’s dignity rather than expose them to discrimination or exploitation.
The real question is not whether pharmacogenomics has benefits, as it clearly does, but how to make those benefits fair. To start, only tests with strong scientific evidence should be used widely. Patients should not be offered tests that are not proven to help, because that wastes resources and hurts trust. Access also has to be addressed. Insurance companies need to consistently cover pharmacogenomic testing, and public programs should step in where insurance does not. Without this, testing will remain mostly for the wealthy. Geography should not be the deciding factor either. Programs that connect rural clinics to large hospitals through telehealth or “hub-and-spoke” systems can help close the gap.12 From a CIT lens, this is an issue of solidarity and the preferential option for the poor, a core Catholic principle that says those who are most vulnerable should be prioritized. If pharmacogenomics can prevent suffering, then moral responsibility demands we extend it to those most likely to be left behind. Research must also become more diverse. If studies only include people of European ancestry, the results will not be accurate for other groups.13 True justice in science requires inclusion. Informed consent must also improve. Most patients do not read long, legalistic consent forms. They need clear explanations of what testing means and how their data will be used. CIT emphasizes the virtue of prudence, which in this context means helping people make wise, informed choices that respect their autonomy. Ethical medicine should empower, not confuse, the patient.

Once the problems are clear, it is not enough to just point them out. Action is needed. Governments and insurers have a responsibility to make testing available. If it is left to market forces, it will mostly serve people who already have advantages. Public investment can help spread access more quickly, just like with vaccines and other medical advances. On the international level, wealthy countries can work with low- and middle-income countries to share resources and knowledge so the gap does not grow wider. Healthcare systems show that it is possible to expand pharmacogenomics. The Veterans Health Administration in the U.S. has built one of the largest programs, making testing available to veterans across the country. The Mayo Clinic has also integrated testing into electronic health records, giving doctors automatic decision support when prescribing.14 These examples prove that it can be done when organizations decide to prioritize it. In the CIT, this is where the virtue of responsibility comes in. Knowledge brings obligation. CIT teaches that science and faith are not opposed; they work together when directed toward the common good. The Pontifical Academy for Life (2019) stresses that scientific progress must never be separated from moral responsibility.15 Pharmacogenomics, like all technology, should be guided by compassion and justice, ensuring that innovation uplifts the whole human family rather than serving only a few. Doctors, pharmacists, and nurses also have responsibilities. They need training so they know how to use pharmacogenomic results correctly. Genetic counselors can help patients understand not just the medical side but also the ethical issues, like privacy and consent. This connects with the Catholic virtue of care for the whole person, reminding us that healthcare is about both body and soul. Technology can also help spread access. Telehealth can connect rural patients with experts in bigger hospitals. Hub-and-spoke systems let smaller clinics send samples to larger labs, so even communities without local resources can take part. On a global level, groups like the World Health Organization and Catholic healthcare networks both stress the same thing: fairness in access is a moral duty, not an optional improvement.
Pharmacogenomics has the potential to transform healthcare by making treatment safer, more effective, and more personal. The science is strong, and the benefits are already visible in cases like warfarin dosing, abacavir hypersensitivity, and cancer therapy. But access is still limited, mostly to wealthy hospitals and patients who can afford it. If nothing changes, pharmacogenomics could become another example of science that increases inequality. The CIT calls us to evaluate such innovations through the lens of justice, solidarity, prudence, and human dignity. It teaches that science is a gift meant to serve all, especially the poor and vulnerable. When applied wisely, pharmacogenomics can fulfill this vision by reducing suffering and promoting the common good. But that will only happen if society acts with moral courage and responsibility. If equity is made a priority, pharmacogenomics could live up to its promise and become one of the most important medical advances of our time, one that reflects not only scientific progress but also moral integrity.
- Mancinelli, Linda, Monica Cronin, and Wolfgang Sadée. “Pharmacogenomics: The Promise of Personalized Medicine.” AAPS PharmSci 2, no. 1 (2000): E4. https://doi.org/10.1208/ps020104. ↵
- Salari, Pooneh, and Bagher Larijani. “Ethical Issues Surrounding Personalized Medicine: A Literature Review.” Acta Medica Iranica 55, no. 3 (2017): 209–217. https://acta.tums.ac.ir/index.php/acta/article/view/6215. ↵
- Johnson, Julie A., Kristin E. Caudle, Li Gong, Michelle Whirl-Carrillo, C. Michael Stein, Stuart A. Scott, Ming-Ta Michael Lee, Brian F. Gage, Scott E. Kimmel, M. A. Perera, Munir Pirmohamed, Teri E. Klein, and Larisa H. Cavallari. “Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines for CYP2C9 and VKORC1 Genotypes and Warfarin Dosing.” Clinical Pharmacology & Therapeutics 102, no. 3 (2017): 397–404. https://doi.org/10.1002/cpt.668. ↵
- Phillips, Elizabeth J., Simon Mallal, and Rebecca K. Pavlos. “Genetic Risk Factors for Hypersensitivity Reactions to Abacavir: A Systematic Review and Meta-Analysis.” Pharmacogenomics 16, no. 11 (2015): 1161–1177. https://doi.org/10.2217/pgs.15.80. ↵
- Budnitz, Daniel S., Maribeth C. Lovegrove, Nadine Shehab, and Cathleen L. Richards. “Emergency Hospitalizations for Adverse Drug Events in Older Americans.” New England Journal of Medicine 365, no. 21 (2011): 2002–2012. https://doi.org/10.1056/NEJMsa1103053. ↵
- Fragala, Matthew S., Elizabeth J. Oesterle, Ann J. O’Rourke, and Christine E. Hawley. “Clinical and Economic Outcomes of a Pharmacogenomics-Enriched Comprehensive Medication Management Program.” The Pharmacogenomics Journal 24, no. 1 (2024): 1–12. https://doi.org/10.1038/s41397-024-00350-1. ↵
- Pontifical Academy for Life. Roboethics: Humans in the Age of Automation. Vatican City: Libreria Editrice Vaticana, 2019. https://www.academyforlife.va. ↵
- Mancinelli, Linda, Monica Cronin, and Wolfgang Sadée. “Pharmacogenomics: The Promise of Personalized Medicine.” AAPS PharmSci 2, no. 1 (2000): E4. https://doi.org/10.1208/ps020104. ↵
- Salari, Pooneh, and Bagher Larijani. “Ethical Issues Surrounding Personalized Medicine: A Literature Review.” Acta Medica Iranica 55, no. 3 (2017): 209–217. https://acta.tums.ac.ir/index.php/acta/article/view/6215. ↵
- Magavern, Elizabeth F. “Equal Access to Pharmacogenomic Testing: The Ethical Challenge.” British Journal of Clinical Pharmacology 89, no. 4 (2023): 1234–1242. https://doi.org/10.1111/bcp.15689. ↵
- Yunta, Eva R. “The Application of Bioethical Principles in the Use of Pharmacogenomics in Person-Centered Medicine.” Medical Research Archives 10, no. 7 (2022): 2881. https://esmed.org/MRA/mra/article/view/2881. ↵
- Paetznick, Courtney V., David E. Lanfear, Kathryn Drozda, Larisa H. Cavallari, and Deepak Voora. “The Intersection Between Pharmacogenomics and Equity.” Frontiers in Pharmacology 14 (2023): 953142. https://doi.org/10.3389/fphar.2022.953142. ↵
- Roman, Yvette M., Justin C. Lin, Kristina Lau-Min, and M. A. Perera. “Pharmacogenomics and Health Disparities: The Need for Diversity and Inclusion.” Frontiers in Genetics 14 (2023): 1233045. https://doi.org/10.3389/fgene.2023.1233045. ↵
- Bielinski, Sarah J., Janet E. Olson, Jyotishman Pathak, et al. “Preemptive Genotyping for Personalized Medicine: Design of the Right Drug, Right Dose, Right Time—Using Genomic Data to Individualize Treatment Protocol.” Mayo Clinic Proceedings 92, no. 4 (2017): 638–651. https://doi.org/10.1016/j.mayocp.2017.01.018. ↵
- Pontifical Academy for Life. Roboethics: Humans in the Age of Automation. Vatican City: Libreria Editrice Vaticana, 2019. https://www.academyforlife.va. ↵