Introduction
Since the completion of the Human Genome Project (HGP) in 2003, efforts to sequence larger genomes were in high demand, as there was a need for affordable and accurate genome sequencing. The creation of next generation sequencing (NGS) met this demand by allowing millions of DNA fragments to be sequenced at once, replacing Sanger sequencing, which could handle only one fragment at a time. These advances in genomic sequencing technology, its cost effectiveness, and its open sharing of data have supported the advances in various fields of medicine and are being applied more readily in basic and clinical research settings (Sharman, n.d.). According to Vassy et al. (2018), tens of thousands of individuals have already received genome sequencing results through clinical or research channels, and programs including the 100,000 Genomes Project in the United Kingdom, the Precision Medicine Initiative All of Us Research Program in the United States, and others are poised to increase this number by millions in the near future. As a result, primary care physicians (PCPs) must navigate the complexities of genome sequencing, including identifying secondary or incidental findings (IFs)—genetic results that are unrelated to the condition or reason for which the sequencing was originally performed (Vassy et al., 2018).

Several questions arise as more IFs occur in genomic sequencing, such as: What are the consequences of sharing secondary findings? What are the consequences of not sharing? And how do we define the spectrum of risk associated with an incidental finding (IF)? As cases of these incidental findings (IFs) continue to increase, there is ethical debate on whether PCPs should be obligated to share all genomic testing results with their patients. The main issues surrounding this moral dilemma involve the primary care physician’s duty and the patient’s autonomy in deciding whether to learn about a secondary finding they did not originally consent to receive. These questions and dilemmas will be examined to clarify the challenges surrounding the disclosure of secondary findings in genomic research.
Obligation to Disclose Genomic Results
Even though full patient autonomy in consenting to genomic secondary findings seems ethically sound, the physician’s responsibilities complicate this issue. These responsibilities include the ethical and professional obligation to act in the best interest of the patient, preventing harm and promoting the well-being of the patient, and strengthening the physician-patient relationship. Other reasons include legal liability concerns, public health and family benefits, and the fact that most patients typically lean in to wanting disclosure on IFs.
A case that resembles the positive impact of incidental findings involves a child with cerebral adrenoleukodystrophy (cALD) who needed a hematopoietic stem cell transplantation (HSCT). Cerebral adrenoleukodystrophy is a genetic, progressive neurological disorder that can lead to difficulty walking, learning disabilities, inability to perform activities, and seizures (Rathore, 2021). To ensure the treatment plans suited the child, whole-exome and whole-genome sequencing (WES/WGS) were utilized and revealed an incidental diagnosis of cystic fibrosis (CF). Although CF is rare in HCST patients, the IF helped prevent an increase in risk of airway complications by allowing the team to carefully balance the use of busulfan, a drug essential essential for cALD treatment but can cause lung toxicity. The parents were grateful that these findings provided them with a deeper understanding of their son’s condition and that it helped them understand the implication of their son’s health. If the IF had not been disclosed, serious complications would have arisen, and the child would have gone through unnecessary suffering (Adriel et al., 2025).
When analyzing an individual’s genome, their genetic makeup consists of genes that were inherited from their parents and will eventually be handed down to their potential children. This means genomic IFs generated in clinical settings may have potential and direct clinical implications or utility for the patient and his/her family’s health, or useful for reproductive health or for future planning. Thus, making the return of IFs, access to treatment, and follow up in clinical settings an obligatory clinical duty (AlFayyad et al., 2021).
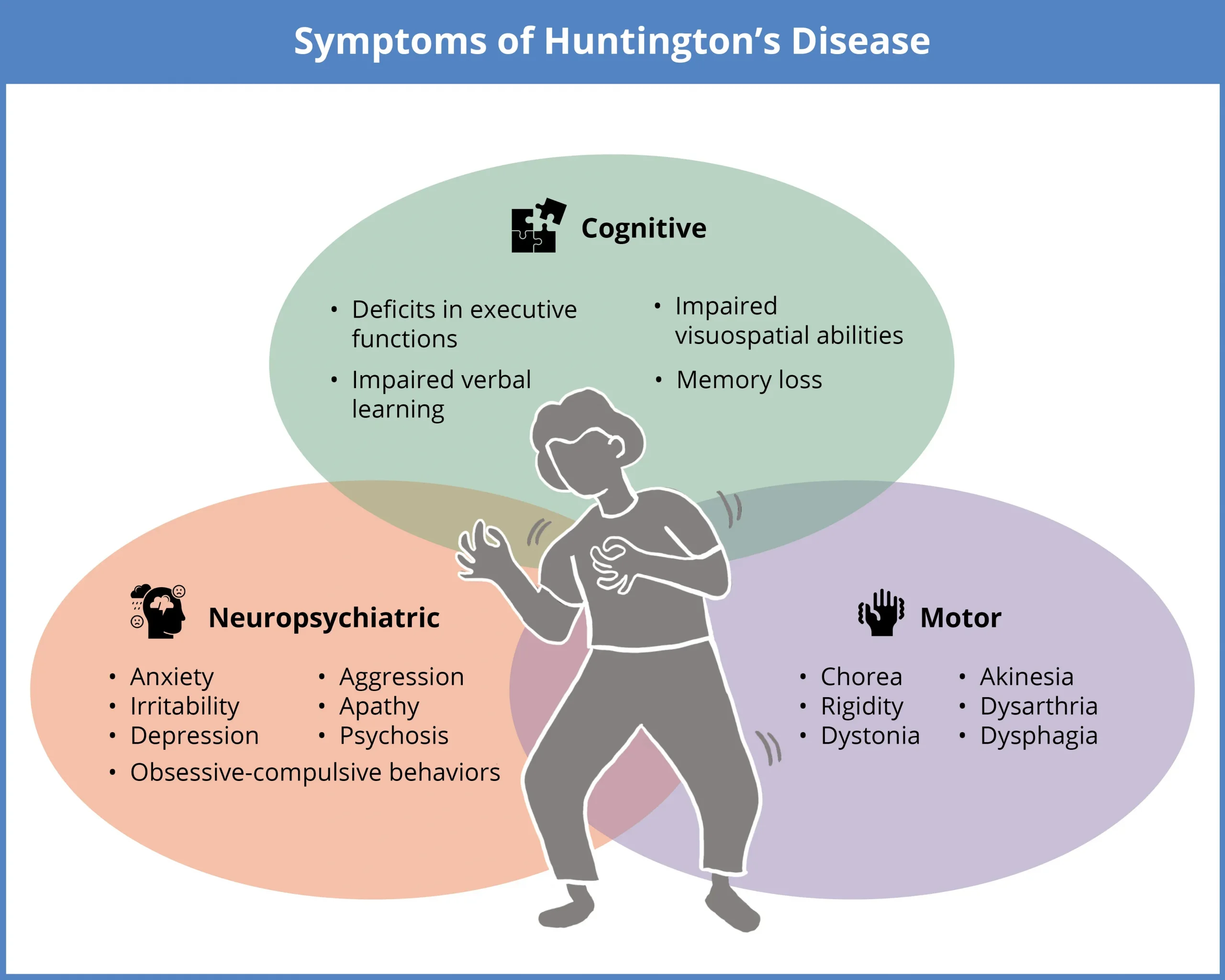
A relevant ethical tension can be seen in the lawsuit brought against a London hospital by a woman whose father’s doctor failed to inform her of her risk of Huntington’s disease. Huntington’s is a rare disease that causes nerve cells in the brain to decay over time and affects a person’s movements, thinking ability, and mental health (Mayo Clinic, 2024). In this case, the woman’s father was diagnosed with this disease in 2009 but refused to let doctors inform his family. The daughter did not find out about this condition until after she had given birth and found out that she tested positive for Huntington’s and that her daughter had a 50% chance of also being affected. The woman said if she had known prior, she would not have become a mother (Mackle, 2018). Although this example was not a consequence of failing to inform a patient of an IF, the effects are still the same. The lack of transparency of these results caused distress in this individual and prevented her from getting medicinal help sooner.
Regarding the spectrum of risk associated with secondary findings, penetrance data helps decide whether an IF should be included in the overall result list that the physician will have to report back to the patient. This is important because penetrance indicates the likelihood that an individual carrying a specific pathogenic variant will develop the disease, helping to determine the level of risk. Although it is a good method on determining whether an IF should be included in an individual’s results, it is important to note that there is no threshold for inclusion in the findings. Such choices are based on multiple factors, not penetrance alone (Gordon et al., 2024). Nonetheless, depending on the severity of the disease and the penetrance, a majority of physicians would return the IFs if the risk of disease was high (AlFayyad et al., 2021).

Another way to identify the severity of a secondary finding is by using the American College of Medical Genetics and Genomics (ACMG) guidelines. According to the ACMG, genetic variants can be categorized as pathogenic, likely pathogenic, of uncertain significance (VUS), likely benign, or benign (Richards et al., 2015). This guideline helps clinicians confidently identify whether a variant is linked to a disease. For example, a variant labeled as “pathogenic” would alert the physician and typically warrant a disclosure with the patient, while a VUS would not be reported until further evidence clarifies its severity. Guidelines such as these, as well as genetic results and penetrance data are important when deciding on sharing such findings with the patient.
Lastly, several studies have shown that most patients and research participants prefer to be informed of any incidental findings (IFs) identified by physicians or investigators when analyzing their genome, as they believe this information would be in their best interest (Cheung et al., 2022; Etchegary et al., 2022; Best et al., 2022). From the examples provided in this section, secondary findings are useful in preventing harm and promoting the well-being of the patient, and can offer public health and family benefits. They also show the consequences that could or could have occurred if secondary findings were not disclosed to the patient.
Challenges in Returning Genomic Results
While the disclosure of incidental findings can promote the health of the patient and offer them more opportunities in making informed decisions about their health, there are still challenges with respecting the autonomy of the individual. For some individuals, learning about IFs can trigger severe distress and anxiety, potentially leading them to seek unnecessary or invasive medical interventions that can carry risks. Such results can also affect family dynamics, cause stigma, or raise concerns about employment and insurance.
“We may be creating a lot of disease here where there isn’t any. So, that’s the downside of this too. Parents who have [a result] that is a potential disease in the future and not even a definite disease in the future, may see that child differently, treat them differently. They never really understand that you said, ‘but it’s okay’ (Pediatric cardiologist 25).”

In this statement, a pediatric cardiologist shared their personal experience with sharing IFs to various families regarding their children. No matter what the pediatrician had said to comfort them or inform them that their situation would be fine, the families could not get past what the physician had revealed to them. This scenario shows the challenges doctors must face when sharing IFs by showing that a “positive” finding can be wrongly treated as a medical diagnosis even though the person involved has no symptoms or actual disease. The same worry applies to “negative” findings since they can offer false reassurance, causing patients to assume they are free of risk even though genetics is not the only factor when dealing with a disease (Pet et al., 2019).
“You told me I had this cardiomyopathy gene; I’ve never developed cardiomyopathy but I owe $5,000 in deductible each year because I was recommended to get an MRI and then when I got the MRI my IV infiltrated and I had a bad infection (Patient 05).”
In this scenario, pediatric cardiologist 05 shares another major concern physicians have about reporting IFs which is the risk of unnecessary medical intervention and its consequences. Although the patient’s health was prioritized and the physician did their duty in informing them, the patient ended up suffering a lot more than if they were not told about the IF (Pet et al., 2019).
Other major issues also arose in the communication between researchers and physicians and who should take responsibility for the results. Several physicians felt that they should not be held responsible for genomic testing because it involved knowledge that was out of their field. They also felt that certain responsibilities such as genetic counseling and further genomic testing should be passed on to genetic specialists and counselors. However, physicians felt that even though there were risks associated with informing their patients about IFs, it was still their duty as physicians to report results regardless of who ordered the tests (Pet et al., 2019; Rahimzadeh et al., 2014a).
When considering the level of risk associated with incident findings (IFs), it is clear that assessing risk involves more than relying on penetrance data. The actual risk to an individual can be influenced by multiple factors, including environmental exposures, lifestyle choices, mental health, and other genetic factors. Furthermore, the presence of a disease-causing mutation does not necessarily mean the disease will manifest. Thus, evaluating clinical context and family history is essential for determining risk.
Finding A Responsible Approach
Although each side presents valid points regarding the advantages and risks of sharing incidental findings (IFs), it remains important to identify a solution that balances both interests. As stated by Bowling et al. (2022), several international groups (European Society for Human Genetics (ESHG), the Canadian College of Medical Geneticists (CCMG), and EuroGentest), all recommend targeted data analysis to reduce SF and/or IF identification, but suggest laboratories provide patients with the option to receive such findings. By using targeted data analysis, the physician is able to focus more on the primary findings initially seeked out by the patient without the stress of encountering other IFs that could potentially come up from a non-targeted analysis. This approach preserves both physician integrity and patient autonomy by avoiding unnecessary incidental findings.

Another potential solution would be for physicians and researchers to implement a system in which communication of consent occurs prior to genomic sequencing regarding IFs. Understanding what is important to the patient allows clinicians to respect patient autonomy while still fulfilling their duty as caretakers. Additionally, providing genetic counselors and genetic specialists also helps ensure that the patient is being properly helped and that the information regarding their genome is being accurately interpreted. By doing either of these approaches, the risk of harm from IFs can be significantly reduced, allowing physicians, patients, and researchers to remain ethically protected.
Connection to Catholic Intellectual Tradition
In navigating this ethical dilemma, it is crucial to find a resolution that considers both sides and consistently honors the Catholic Intellectual Tradition’s principles of human dignity, solidarity, and stewardship. Respecting an individual’s human dignity means recognizing that individuals are more than their genetic data and deserve autonomy in their decision regarding disclosure of results. Solidarity calls for the unity of healthcare professionals and researchers to act with compassion and responsibility, ensuring that disclosure of such findings respects the patient’s preferences and promotes their health and safety. The principle of stewardship can be implemented by protecting privacy, avoiding misuse, and promoting care that reflects moral responsibility toward human life. Addressing these core values reinforces the physician’s duty to manage incidental findings in ways that respect the patient’s dignity, autonomy, and health.
Conclusion
Ultimately, finding the balance in physician responsibilities and patient preferences is essential to ethical management of incidental findings. While most individuals believe that learning about any secondary finding is beneficial regardless of the level of risk, some may be harmed by knowing. The same can be said for physicians, who are often overwhelmed by incidental findings and may struggle to effectively guide their patients due to gaps in their knowledge. It is also important to note that incidental findings are not inherently bad, as they can provide helpful clinical feedback and potentially save lives.
As technology continues to advance and more individuals begin to sequence their genomes, it is important to continue searching for solutions revolving around the ethical dilemma behind incidental findings. When developing and implementing such solutions, the interests of both physicians and patients must come first, as both have been affected by the rise in incidental findings. The solution should enable physicians to prioritize their patients’ health and preferences, while ensuring that patients feel confident they will be supported and guided through their genetic results.
Citations
Adriel, J., Tan, P. L., Lin, J. B., Tay, S. K.-H., & Chin, H.-L. (2025). Case report: Incidental diagnosis of cystic fibrosis via whole genome sequencing alters HSCT planning in a child with cerebral X-linked adrenoleukodystrophy. Frontiers in Pediatrics, 13. https://doi.org/10.3389/fped.2025.1650645
AlFayyad, I., Al-Tannir, M., Abu-Shaheen, A., & AlGhamdi, S. (2021). To disclose, or not to disclose? Perspectives of clinical genomics professionals toward returning incidental findings from genomic research. BMC Medical Ethics, 22(1). https://doi.org/10.1186/s12910-021-00670-y
Best, M. C., Butow, P., Savard, J., Jacobs, C., Bartley, N., Davies, G., Napier, C. E., Ballinger, M. L., Thomas, D. M., Biesecker, B., Tucker, K. M., Juraskova, I., Meiser, B., Schlub, T., & Newson, A. J. (2022). Preferences for return of germline genome sequencing results for cancer patients and their genetic relatives in a research setting. European Journal of Human Genetics, 30(8), 930–937. https://doi.org/10.1038/s41431-022-01069-y
Bowling, K. M., Thompson, M. L., Kelly, M. A., et al. (2022). Return of non-ACMG recommended incidental genetic findings to pediatric patients: Considerations and opportunities from experiences in genomic sequencing. Genome Medicine, 14, 131. https://doi.org/10.1186/s13073-022-01139-2
Cheung, F., Birch, P., Friedman, J. M., Elliott, A. M., & Adam, S. (2022). The long-term impact of receiving incidental findings on parents undergoing genome-wide sequencing. Journal of Genetic Counseling, 31(4), 887–900. https://doi.org/10.1002/jgc4.1558
Etchegary, H., Pullman, D., Simmonds, C., & Rahman, P. (2022). Public interest in unexpected genomic findings: A survey study identifying aspects of sequencing attitudes that influence preferences. Journal of Community Genetics, 13(2), 235–245. https://doi.org/10.1007/s12687-022-00577-0
Gordon, A. S., Lee, K., Abul-Husn, N. S., Amendola, L. M., Brothers, K., Chung, W. K., Gollob, M. H., Harrison, S. M., Hershberger, R. E., Richards, C. S., Stewart, D. R., Martin, C. L., & Miller, D. T. (2024). Consideration of disease penetrance in the selection of secondary findings gene-disease pairs: A policy statement of the American College of Medical Genetics and Genomics (ACMG). Genetics in Medicine, 26(7), 101142. https://doi.org/10.1016/j.gim.2024.101142
Mackle, E. (2018, December 3). Woman sues UK hospital over Huntington’s inheritance | PET. PET. https://www.progress.org.uk/woman-sues-uk-hospital-over-huntingtons-inheritance/
Mayo Clinic. (2024, April 25). Huntington’s disease. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
Pet, D. B., Holm, I. A., Williams, J. L., Myers, M. F., Novak, L. L., Brothers, K. B., Wiesner, G. L., & Clayton, E. W. (2019). Physicians’ perspectives on receiving unsolicited genomic results. Genetics in Medicine, 21(2), 311–318. https://doi.org/10.1038/s41436-018-0047-z
Rahimzadeh, V., Avard, D., Sénécal, K., Knoppers, B. M., & Sinnett, D. (2014a). To disclose, or not to disclose? Context matters. European Journal of Human Genetics, 23(3), 279–284. https://doi.org/10.1038/ejhg.2014.108
Rathore, G. (2021, July). Cerebral adrenoleukodystrophy. Child Neurology Foundation. https://www.childneurologyfoundation.org/disorder/cerebral-adrenoleukodystrophy/
Richards, S., Aziz, N., Bale, S., Bick, D., Das, S., Gastier-Foster, J., Grody, W. W., Hegde, M., Lyon, E., Spector, E., Voelkerding, K., Rehm, H. L., & ACMG Laboratory Quality Assurance Committee (2015). Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genetics in medicine : official journal of the American College of Medical Genetics, 17(5), 405–424. https://doi.org/10.1038/gim.2015.30
Sharman, Dr. S. (n.d.). The evolution of DNA sequencing technology: Part 2. Genomics Education Partnership. https://thegep.org/sequencing/evolution-of-dna-sequencing-part-2/
Vassy, J. L., Davis, J. K., Kirby, C., Richardson, I. J., Green, R. C., McGuire, A. L., & Ubel, P. A. (2018). How primary care providers talk to patients about genome sequencing results: Risk, rationale, and recommendation. Journal of General Internal Medicine, 33(6), 877–885. https://doi.org/10.1007/s11606-017-4295-4


