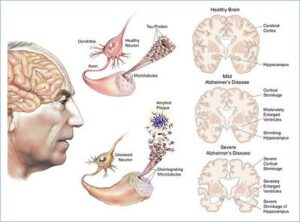
As the number of elderly people increases worldwide, the effects of impairments related to age, such as dementia, become more relevant. Dementia results in cognitive dysfunction, which can impair judgement, impair decision making, affect communication, and impede or prevent independent life.1 Although dementia can be diagnosed in many different stages, the main hallmark is cognitive decline seen with memory and higher executive function.1 The cause of this decline can be a result of multiple factors dependent on site and progression of lesions and neuron loss.1 Dementia may present in many different forms, each portraying their own unique symptoms. The different forms include Alzheimer’s disease (AD), frontotemporal dementia, progressive aphasias, Lewy-body dementia, and posterior cortical atrophy, among others.1 This article will focus on AD with the primary symptom being impairment of recent memory. Figure 1 depicts the brain regions that are typically involved with mild to severe stages of AD.
Alzheimer’s disease not only affects memory, but it can also affect one’s mood, quality of life, daily activities, and one’s need for care.10 There are many drugs being tested for the treatment of this disease, although none of them have been able to reverse the disease. The four drugs that are currently on the market for the treatment of Alzheimer’s disease are Donepezil, Galantamine, Rivastigmine, and Memantine.10 The first three drugs are acetylcholinesterase inhibitors for the treatment of mild to severe Alzheimer’s disease while the fourth drug is an NMDA receptor antagonist for the treatment of moderate to severe Alzheimer’s disease.10 Acetylcholinesterase is an enzyme that breaks down acetylcholine as nerve junctions. The inhibition of this enzyme leads to a higher concentration of acetylcholine in the brain and better communication between the nerve cells. NMDA receptors are important for synaptic plasticity and survival of neurons, but excessive activity, as seen with AD, causes excitotoxicity and promotes cell death. The use of receptor antagonists helps to reduce the excessive activity leading to survival of the neurons, even if neural plasticity is diminished.13 Like every drug on the market there are side effects, but without the reversal of the disease some people have opted to manage the disease in other ways. Neuroplasticity has gained traction in the research community as a possible treatment for dementia without the use of traditional drugs.
Neuroplasticity is the ability of the brain to “rewire” itself by establishing new neural connections. This rewiring could be the consequence of injury, developmental or environmental changes, or changes caused by sensory input.8 In the case of injury, the brain can reroute tasks that were normally associated with one area to a completely unrelated area in the brain. Neuroplasticity is also seen with establishing new skills to improve one’s memory. As people begin to age, a decline is seen in their memory, attention, and learning skills.8 Although, the ability for the brain to remain plastic and reroute connections does not degrade with age. Neuron growth can be stimulated through specific exercises on sensory input, movement, and cognitive patterns.
Neuroplasticity is a promising as treatment for both the patient and their family members. A study published in 2010 by Kolanowski, et al. looked at delirium superimposed on dementia (DSD) and certain activities used to facilitate plasticity.16 For individuals with dementia, delirium occurs in over half of the hospitalized adults, compounding their physical and cognitive burdens that were already present. The article defined delirium as a “state of confusion characterized by an acute onset, alteration of consciousness, change in cognition, fluctuating course, and reduced attention.”16 As individuals age their cognition declines which is correlated with diminished neurogenesis, the growth of nervous tissue, and plasticity in the hippocampus, the center of emotion and memory. Delirium could be caused by many different problems, be it a decrease in blood flow to various parts of the brain, a brain lesion, or derangements of neurotransmitters.16 It may not be obvious how dementia is related to delirium, but dementia is the strongest risk factor of delirium with the primary deficit being attention. In regard to neuroplasticity, the brain can change through activity-based neuroplasticity through the response of experience or activity.
There are two ways that the brain can be modified. These include plasticity of existing neurons or neurogenesis. The use of activity-based neuroplasticity is continued through adulthood when neurogenesis begins to cease. Activities to help develop the brain include learning and problem-solving challenges, exercise, and sensory stimulation. Engaging in these activities are beneficial for individuals with dementia to help engage their brain to produce positive behavioral and cognitive change. Specifically, long-term regular exercise shows benefit to reducing dementia progression.19The sustained exercise that is being defined is aerobic exercise that increases the heart rate and need for oxygen lasting at least 20-30 minutes per session. This type of exercise is known as cardiovascular fitness and can be completed through walking, running, home activities, gym, or health club routines.19 Analysis of 29 randomized controlled trials indicated that aerobic exercise significantly improved cortical connectivity, in the regions associated with memory.1922 Significant improvements were also evident when patients were given cognitive tasks. Sustained exercise in patients with Alzheimer’s disease also saw a reduction in the risk of morality.19 Exercise is an easy task that can be completed by individual’s suffering from AD with the benefits helping their mind and creation of a healthier body.
Exercise has shown promising improvements to the cognitive effects of dementia, but some patients are unable to engage in these activities due to health problems. Alzheimer’s disease is one of the most damaging forms of dementia and is very common in an aging population where physical exercise may not be feasible due to barriers like back pain, sore knees, heart conditions, or lung disorders. The current care for Alzheimer’s disease is cholinergic and glutamatergic drugs which contain many adverse side effects.24 Instead of the use of exercise, neuroplastic treatment through repetitive non-invasive brain stimulation can help slow down cognitive decline and enhance neuronal activity.
Repetitive transcranial magnetic stimulation (rTMS) is a noninvasive brain stimulation method to promote neuroplastic changes in patients with Alzheimer’s disease.24 rTMS is a painless procedure that generates a magnetic pulse through a stimulated coil that is placed on a patients head.26 A transient electric field is produced underneath the surface that causes depolarization of the neurons in the cerebral cortex.26 Patients who have mood disorders and depression can be influenced by rTMS to repair these processes. Specifically, long term potentiation (LTP) is the best target for this treatment since it is linked to cognitive function and is the most widely proposed mechanism for memory storage.2624 LTP involves the strengthening of neuronal synapses leading to long-lasting transmission in neuronal signals. In the early stages of Alzheimer’s disease, cortical plasticity is impaired, affecting one’s verbal memory. The use of rTMS on LTP cortical plasticity could help to reduce the progression of the disease.24 The best course of treatment may involve long term use of these methods to target the prefrontal cortex for the improvement of cognitive function.24 With research continuing in this area, the full effects of this treatment are still unknown, but the results are promising. Through this research, it is also evident that Alzheimer’s disease does not have to be targeted specifically to improve cognitive function. If patients are diagnosed with other neurological conditions, targeting these conditions could have a positive impact on the cognitive problems they may be experiencing.
A study that went in depth on the use of rTMS treatment along with cognitive training (CT) found improvement of AD symptoms that was associated with disease progression and level of education. Adding rTMS with cognitive training is used to enhance neuroplasticity by combining exogenous and endogenous stimulation.26 In this study, only the left dorsolateral prefrontal cortex, involved in executive function and control of cognitive processes, was stimulated and a face-name memory test was conducted.2634 They conducted the research through two groups, one where patients received rTMS with CT and one where patients only received CT.26 In the patients who received the rTMS, it was administered before cognitive training to “prime” their brain to increase the efficiency of face-name associative memory.26 The results of the face-name memory tests are shown in Figure 3 after 4 weeks of treatment was completed.
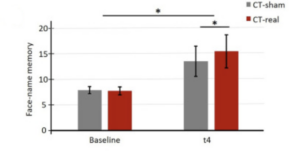
The results from the study showed CT sessions alone were effective in improving face-name associative memory along with an enhancement in improvement with rTMS.26 Nonetheless, this improvement was associated with the severity of the disease and education, thus limiting the effect that the treatment could have on patients.26 Based on these results, if AD is diagnosed early, then CT treatment with rTMS is a viable option to replace the use of medication. To achieve the best results during treatment, the study advised to propose treatment with this method as early as possible before neuronal loss is seen.26 This method can cause neuroplastic long term potentiation changes in the brain, reducing the life changing effects of AD, but there are limits to this method. It is heavily dependent on the stage of AD and the amount of education the patient has. Having a higher education allows individuals to link new knowledge with stored knowledge which can demonstrate a faster treatment of symptoms and act against AD progression. This does not mean treatment cannot be conducted on people with less education, the results may not be as evident.
The rise of neuroplasticity as treatment for dementia is showing promising results by increasing cognitive ability. Through long term exercise or stimulation of neuronal pathways with rTMS to initiate neuroplasticity in the brain, patients can find relief from the life changing conditions of their disease. Even though dementia is not yet reversible, patients whose memory and cognitive ability is declining can still lead more fulfilling lives than they would have been able to otherwise. Continued research is still being conducted on the benefits of neuroplasticity for treatment, but current results are promising towards the field of neurodegenerative diseases.
- Wolf, C., Rosen, J. A., Constas, D., & Mermelstein, H. (2017). Distinguishing dementia from mental illness and other causes of decline New York State Bar Association Journal, 89(1), 22-27. ↵
- Wolf, C., Rosen, J. A., Constas, D., & Mermelstein, H. (2017). Distinguishing dementia from mental illness and other causes of decline New York State Bar Association Journal, 89(1), 22-27. ↵
- Wolf, C., Rosen, J. A., Constas, D., & Mermelstein, H. (2017). Distinguishing dementia from mental illness and other causes of decline New York State Bar Association Journal, 89(1), 22-27. ↵
- Wolf, C., Rosen, J. A., Constas, D., & Mermelstein, H. (2017). Distinguishing dementia from mental illness and other causes of decline New York State Bar Association Journal, 89(1), 22-27. ↵
- Puma, J. L. (2021, September 21). World Alzheimer’s Day 2021: The stages of alzheimer’s disease. Mountainside Medical Equipment. Retrieved March 30, 2023, from https://www.mountainside-medical.com/blogs/medical-supplies/world-alzheimers-day-2021-the-stages-of-alzheimers-disease. ↵
- U.S. Department of Health and Human Services. (2017, May 16). What happens to the brain in alzheimer’s disease? National Institute on Aging. Retrieved March 11, 2023, from https://www.nia.nih.gov/health/what-happens-brain-alzheimers-disease. ↵
- U.S. Department of Health and Human Services. (2017, May 16). What happens to the brain in alzheimer’s disease? National Institute on Aging. Retrieved March 11, 2023, from https://www.nia.nih.gov/health/what-happens-brain-alzheimers-disease. ↵
- Sheposh, R. (2023). Neuroplasticity. Salem Press Encyclopedia of Health. ↵
- “Healthy Brain and Severe AD Brain” by National Institutes of Health (NIH) is marked with Public Domain Mark 1.0. To view the terms, visit https://creativecommons.org/publicdomain/mark/1.0/?ref=openverse. ↵
- Piscopo, P., Crestini, A., Rivabene, E., Ancidoni, A., Lo Giudice, M., Corbo, M., Vanacore, N., & Lacorte, E. (2022, August 27). A systematic review on drugs for synaptic plasticity in the treatment of dementia. Ageing Research Reviews. Retrieved March 28, 2023, from https://www.sciencedirect.com/science/article/pii/S1568163722001684?via%3Dihub ↵
- Piscopo, P., Crestini, A., Rivabene, E., Ancidoni, A., Lo Giudice, M., Corbo, M., Vanacore, N., & Lacorte, E. (2022, August 27). A systematic review on drugs for synaptic plasticity in the treatment of dementia. Ageing Research Reviews. Retrieved March 28, 2023, from https://www.sciencedirect.com/science/article/pii/S1568163722001684?via%3Dihub ↵
- Piscopo, P., Crestini, A., Rivabene, E., Ancidoni, A., Lo Giudice, M., Corbo, M., Vanacore, N., & Lacorte, E. (2022, August 27). A systematic review on drugs for synaptic plasticity in the treatment of dementia. Ageing Research Reviews. Retrieved March 28, 2023, from https://www.sciencedirect.com/science/article/pii/S1568163722001684?via%3Dihub ↵
- Wang, R., & Reddy, P. H. (2017). Role of Glutamate and NMDA Receptors in Alzheimer’s Disease. Journal of Alzheimer’s disease : JAD, 57(4), 1041–1048. https://doi.org/10.3233/JAD-160763. ↵
- Sheposh, R. (2023). Neuroplasticity. Salem Press Encyclopedia of Health. ↵
- Sheposh, R. (2023). Neuroplasticity. Salem Press Encyclopedia of Health. ↵
- Kolanowski, A. M., Fick, D. M., Clare, L., Therrien, B., & Gill, D. J. (2010). An intervention for delirium superimposed on dementia based on cognitive reserve theory. Aging & Mental Health, 14(2), 232–242. https://doi-org.blume.stmarytx.edu/10.1080/13607860903167853. ↵
- Kolanowski, A. M., Fick, D. M., Clare, L., Therrien, B., & Gill, D. J. (2010). An intervention for delirium superimposed on dementia based on cognitive reserve theory. Aging & Mental Health, 14(2), 232–242. https://doi-org.blume.stmarytx.edu/10.1080/13607860903167853. ↵
- Kolanowski, A. M., Fick, D. M., Clare, L., Therrien, B., & Gill, D. J. (2010). An intervention for delirium superimposed on dementia based on cognitive reserve theory. Aging & Mental Health, 14(2), 232–242. https://doi-org.blume.stmarytx.edu/10.1080/13607860903167853. ↵
- Ahlskog, J. E., Geda, Yonas E,M.D., M.S.C., Graff-Radford, N., & Petersen, Ronald C,P.H.D., M.D. (2011). Physical Exercise as a Preventive or Disease-Modifying Treatment of Dementia and Brain Aging. Mayo Clinic Proceedings, 86(9), 876-84. https://blume.stmarytx.edu/login?url=https://www.proquest.com/scholarly-journals/physical-exercise-as-preventive-disease-modifying/docview/886577831/se-2 . ↵
- Ahlskog, J. E., Geda, Yonas E,M.D., M.S.C., Graff-Radford, N., & Petersen, Ronald C,P.H.D., M.D. (2011). Physical Exercise as a Preventive or Disease-Modifying Treatment of Dementia and Brain Aging. Mayo Clinic Proceedings, 86(9), 876-84. https://blume.stmarytx.edu/login?url=https://www.proquest.com/scholarly-journals/physical-exercise-as-preventive-disease-modifying/docview/886577831/se-2 . ↵
- Ahlskog, J. E., Geda, Yonas E,M.D., M.S.C., Graff-Radford, N., & Petersen, Ronald C,P.H.D., M.D. (2011). Physical Exercise as a Preventive or Disease-Modifying Treatment of Dementia and Brain Aging. Mayo Clinic Proceedings, 86(9), 876-84. https://blume.stmarytx.edu/login?url=https://www.proquest.com/scholarly-journals/physical-exercise-as-preventive-disease-modifying/docview/886577831/se-2 . ↵
- Wang, J. X., Rogers, L. M., Gross, E. Z., Ryals, A. J., Dokucu, M. E., Brandstatt, K. L., Hermiller, M. S., & Voss, J. L. (2014). Targeted enhancement of cortical-hippocampal brain networks and associative memory. Science (New York, N.Y.), 345(6200), 1054–1057. https://doi.org/10.1126/science.1252900. ↵
- Ahlskog, J. E., Geda, Yonas E,M.D., M.S.C., Graff-Radford, N., & Petersen, Ronald C,P.H.D., M.D. (2011). Physical Exercise as a Preventive or Disease-Modifying Treatment of Dementia and Brain Aging. Mayo Clinic Proceedings, 86(9), 876-84. https://blume.stmarytx.edu/login?url=https://www.proquest.com/scholarly-journals/physical-exercise-as-preventive-disease-modifying/docview/886577831/se-2 . ↵
- Koch, G., & Spampinato, D. (2022, January 13). Alzheimer disease and neuroplasticity. Handbook of Clinical Neurology. Retrieved March 11, 2023, from https://www.sciencedirect.com/science/article/pii/B9780128194102000278?via%3Dihub. ↵
- Koch, G., & Spampinato, D. (2022, January 13). Alzheimer disease and neuroplasticity. Handbook of Clinical Neurology. Retrieved March 11, 2023, from https://www.sciencedirect.com/science/article/pii/B9780128194102000278?via%3Dihub. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Koch, G., & Spampinato, D. (2022, January 13). Alzheimer disease and neuroplasticity. Handbook of Clinical Neurology. Retrieved March 11, 2023, from https://www.sciencedirect.com/science/article/pii/B9780128194102000278?via%3Dihub. ↵
- Koch, G., & Spampinato, D. (2022, January 13). Alzheimer disease and neuroplasticity. Handbook of Clinical Neurology. Retrieved March 11, 2023, from https://www.sciencedirect.com/science/article/pii/B9780128194102000278?via%3Dihub. ↵
- Koch, G., & Spampinato, D. (2022, January 13). Alzheimer disease and neuroplasticity. Handbook of Clinical Neurology. Retrieved March 11, 2023, from https://www.sciencedirect.com/science/article/pii/B9780128194102000278?via%3Dihub. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Vahabzadeh, A., & McDougle, C. J. (2014, August 21). Obsessive–compulsive disorder. Pathobiology of Human Disease. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/B9780123864567052138. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵
- Bagattini, C., Zanni, M., Barocco, F., Caffarra, P., Brignani, D., Miniussi, C., & Defanti, C. A. (2020, September 28). Enhancing cognitive training effects in alzheimer’s disease: RTMS as an add-on treatment. Brain Stimulation. Retrieved March 30, 2023, from https://www.sciencedirect.com/science/article/pii/S1935861X20302497. ↵


15 comments
Aaron Astudillo
Thank you for writing this article and congratulations on the nomination. The topic of dementia is often difficult to discuss as it can have such a detrimental impact on families who have a member affected by it. Understanding the role of neuroplasticity in the mental disease of dementia shines a light on it and keeps individuals informed.
Maximillian Morise
This is a very interesting article on the complicated field of neuroscience that you have managed to explain in a very fine and easy to understand way. I congratulate you for your nomination, and I thank you for spreading light on this very complicated subject matter!
Donald Glasen
Congratulations on your nomination! I greatly enjoyed reading your article. It’s always amazing to learn new things. The article was well-written and easy to follow and understand.
D'vaughn Duran
Congratulations on being nominative! This was a great topic to write about because it’s very interesting. Alzheimer’s Disease is often overlooked and it’s very common to have this neurological disease. Many people don’t know anything about this topic because they are not sure about it or don’t have a loved one that has or had it before. This was a well-written article with great information!
Gabriella Parra
Jordyn! Congratulations on your nomination! This article is super interesting because I’m sure many readers know somebody with dementia or Alzheimer’s disease. For me, my grandma has dementia, although it has just started setting in quite recently. I remember she always used to work on problem-solving puzzles. This was mostly because she had nothing else to do, but it is good to know that this was actually good for her health! Great article!
Luke Rodriguez
This was an amazing read! Also, congrats on the nomination! It was well-deserved. The article was well-written and detailed. I enjoyed that you showed the factors that few people know about dementia. Another thing is talking about Alzheimer’s and the many different medicines that were tried and no happy outcomes really intensives the topic.
Alanna Hernandez
Very cool article, you made it pretty easy to follow along. As well as making such a tragic things such as dementia not seem so scary when we have science. I wasn’t aware that doing things that are usually for physical healthy could be beneficial to reducing the progression of dementia. Congratulations on your nomination for best academic explanatory article, it’s well deserved!
Nnamdi Onwuzurike
Congratulations on your nomination! Neuroplasticity, the brain’s ability to reorganize and form new neural connections, has emerged as a promising treatment for dementia. Research has shown that engaging in activities that stimulate the brain, such as learning a new language or playing a musical instrument, can help improve cognitive function and slow the progression of dementia. Understanding the role of neuroplasticity in dementia treatment can help improve the quality of life for individuals with dementia and their caregivers.
Hunter Stiles
This was a really wonderful piece, especially coming from someone whose grandfather has dementia. I’m so happy you’re raising awareness of this illness and providing fresh perspectives. This article was pretty interesting. Even though I had no prior knowledge of the technical jargon, I found the paper to be quite straightforward and easy to understand. Any advancements or study that reveals ways to reduce memory loss’s impact is really intriguing to me as someone who has seen its affects firsthand. I appreciated how you provided a variety of therapy options. It was incredibly thorough and fascinating. Well Done!
Marissa Rendon
This was an amazing article to read! My grandmother’s sister suffered from dementia and her passing was truly a sad one. I am full aware of the effects of memory loss. I truly enjoyed reading the descriptive treatments that can possibly help with dementia. I feel as if dementia is not spoken a lot about and this was truly an amazing article.