Polycystic ovarian syndrome (PCOS) is the most common type of androgen excess disorder for women of childbearing age — accounting for 5-15% of women.1 According to the National Institute of Health, the definition of the syndrome is a complex of clinical and laboratory findings that indicate a specific condition for which a direct cause is distinguished.2 Polycystic Ovarian Syndrome, therefore, is not caused by one specific disorder that happens in the body; rather, it’s a multitude of symptoms that cause the condition. Because of the nature of PCOS, it is commonly underdiagnosed, with as many as 75% of patients with PCOS being unidentified in clinical practice.3 Due to the multifaceted nature of PCOS, there is no “one size fits all” solution to managing it. Since this is a condition that affects so many women, it is important to research, so we can help mitigate the effects it can have in the long term. This paper will go through the case study of patient A and her process of getting diagnosed with PCOS and, eventually, getting treated with metformin.
The Diagnosis of Patient A
Patient A is an 18-year-old female who is having irregular periods, high insulin resistance and an indication of a fatty liver. She has a family history of diabetes and is currently overweight. She has had the presence of Acanthosis nigricans on her neck, armpits, and inner thighs since she was 8 years old. These markings are typically velvety, light-brown-to-black, and it usually can be found on the neck, under the arms or in the groin. This symptom is often associated with diabetes and insulin resistance.4 (Figure 1) When she initially discussed this with her primary care doctor, his immediate thought was to implement a good diet and exercise to combat this because it seemed to be an indicator of pre-diabetes. However, when she came in without having her period for 6 months, he was starting to consider PCOS as a possibility. He referred her to an OBGYN, a women’s health specialist, and the specialist also had the same concerns for patient A.

The doctor discusses with Patient A about the possibility of PCOS and the diagnosis process that will proceed. The Rotterdam Criteria was created to make it easier for medical professionals to identify PCOS in people. The three criteria include oligo-anovulation, hyperandrogenism and polycystic ovaries. For the clinical diagnosis of PCOS, two of the three symptoms need to be fulfilled. The OBGYN goes in depth as to how each criterion is connected and leads to the diagnosis of PCOS.6
The first marker of PCOS is the enlargement of the ovaries due to the development of cysts. Cysts in the ovaries are small egg follicles that do not grow to ovulation and are caused by altered hormone levels. During a normal menstrual cycle, 6-12 follicles mature in the ovaries– producing estrogen to develop the lining of the uterus to build up a fertile environment for a potential pregnancy. As the follicles mature, one of them starts to grow faster and dominate, while the rest of the follicles disintegrate.7 The dominant follicle releases the egg, which then produces progesterone to help maintain the early stages of a pregnancy. or if not fertilized, support menstruation.8 However, if someone has PCOS ovaries’ follicles turn into cysts, enlarging the ovaries, instead of disintegrating and producing an egg. In contrast to the normal process of ovulation, none of the follicles release an egg when someone has PCOS, meaning that the follicles are in a stagnant, in-between state. The alterations PCOS causes consequently result in estrogen being produced and progesterone production being yielded. Clinically, this manifests as Oligovulation or– in simple terms– irregular periods.9 To check for this condition, the provider decides to do a pelvic ultrasound to see if the endometrium of the uterus is abnormally thick or if there is an enlarged uterus due to the excess amount of cysts in the uterus. The pelvic ultrasound detected that the endometrium was normal, but both ovaries were enlarged due to the cysts present in patient A. Therefore, this ultrasound confirms that the first condition in the Rotterdam criteria was met in patient A, leading us closer to a diagnosis.
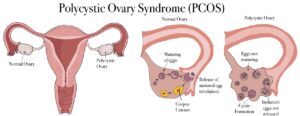
Logically, it is easy to see the connection between enlarged ovaries and the second criterion for being diagnosed with PCOS – Oligovulation. The characterizations of an irregular period are defined as experiencing less than 8 periods in a year and periods being greater than 35 days apart. This definition of oligiovulation is fulfilled by the fact that patient A hasn’t experienced a period in 6 months.10 Although the enlarged uterus is the main component of the ultrasound the provider was looking at to diagnose patient A with PCOS, it is important to monitor the progress of the condition by keeping an eye on the thickness of the endometrial lining. When the uterus does not shed due to a lack of a period, it can cause the endometrial lining to build up, causing possible infertility and/ or endometrial cancer in women. Because patient A’s main concern for coming into the clinic initially was her irregular periods, the importance of checking the thickness of her endometrial lining is emphasized by the provider because of the insulin resistance she is demonstrating currently. It has been observed in a study that women with either insulin resistance or PCOS display higher levels of thickness in the endometrial lining when evaluating the transvaginal ultrasound.11 Regardless of the diagnosis of PCOS, imaging was important in helping patient A solve her issues with irregular menstrual cycles. Hence, for the case of patient A, the second condition for becoming diagnosed with PCOS has been met, calling for an official diagnosis of polycystic ovarian syndrome for that patient.
Even though the patient has already been diagnosed, it is important to check for the third condition, so that the doctors are able to provide comprehensive care. Hyperandrogenism is defined as an excess amount of androgens (a group of sex hormones) in your body.12 Androgens are usually thought of as the male sex hormone; however, In women, androgens normally function to support bone density, muscle mass and sexual function. Testosterone is primarily produced by the ovaries. The clinical manifestations of elevated androgen levels in women include hirsutism (excess hair to grow on certain parts of your body), acne and female pattern hair loss.13 Although none of the clinical manifestations of hyperandrogenism was present in patient A, the laboratory findings indicated the opposite. To check the androgen levels, the OBGYN decided to test the Dhea Sulfate. Providers use DHEAS tests to measure levels of a steroid hormone that your body converts into estrogen and androgens (testosterone).14 Normal Dhea Sulfate levels are usually between 63 – 373 ug according to the range given by the doctor. Patient A scored above the normal range, indicating high testosterone levels. Therefore, using the Rotterdam criteria, it is confirmed that patient A has three out of the three conditions needed to be diagnosed with PCOS.
Other symptoms associated with PCOS that were present in patient A are Nonalcoholic Fatty Liver Disease(NAFLD) and increased susceptibility to depression and anxiety. Nonalcoholic Fatty Liver Disease(NAFLD) is when a person has fat inside their liver, which over time can affect liver function and cause liver injury.15 In regard to depression and anxiety, although the mechanism is not fully understood, it is acknowledged that the imbalance of hormones in the body can cause people with PCOS to be more susceptible to depression and anxiety. In a study that was conducted, it indicated that PCOS patients are up to 8 times more likely to have depression than the control group.16 Polycystic ovarian syndrome is very interconnected and there is a lot that needs to be known to help people like patient A get the treatment they need.
- Metaphormin’s usage for PCOS
As the doctor progresses to the next stage after diagnosis, she considers the standard treatments for PCOS. She discusses with patient A that birth control and/ or metformin are two of the most common treatments for PCOS. Patient A has a familial history of diabetes, so she has heard of metformin in the treatment of diabetes but not for any other conditions. Patient A was initially confused as to how she could take metformin to aid the treatment of her PCOS, especially since she doesn’t have diabetes. The provider explains that metformin is somewhat referred to as a “miracle drug” in the scientific community. Although it is the first line of defense for a lot of diabetic patients, there is growing medical evidence to prove that it also may help lower glucose levels, and weight loss, as well as possible antiaging and cancer benefits.17 Metformin is the generally safer and more effective long‐term treatment option when compared to oral contraceptive pills (OCP).18
Metformin‘s job is to repair the response the body has to insulin. Hyperinsulinemia is having higher amounts of insulin in the blood than what is considered healthy. Hyperinsulinemia is related to type 2 diabetes or other metabolic syndromes.19 Insulin itself is an anabolic hormone, which means it tends to build on each other, making the condition progressively worse. These metabolic syndromes mostly come from lifestyle factors. When you eat food, the body converts it into dietary sugars also known as glucose. Insulin is sent by the pancreas to tell cells to accept the glucose and convert it into energy. When there is insulin resistance in the body, the glucose in the body doesn’t always get paired up with insulin, making the remaining glucose stay in the bloodstream instead of being converted into energy in the cell. Over time, the pancreas continues to make more insulin to compensate for the excessive amount of glucose in the bloodstream until one day the pancreas wears out and can’t produce insulin anymore due to the overuse of the organ.20
Insulin plays a huge role in the production of estrogens, cysts in the ovaries and hyperandrogenism. For example, hyperinsulemia can lead to functional hyperandrogenism, which causes an abnormal increase in luteinizing (LH) hormones. Luteinizing hormones can then stimulate theca cells, which increase the amount of testosterone and other androgens that is produced in the body. Ultimately this whole process results in more severe hyperandrogenism.22 Although the role of hyperinsulinemia in PCOS is a complicated, interconnected system that we are unable to go through sufficiently in this paper, it is important to recognize the important role insulin has in PCOS.
Because of Patient A’s family’s history of diabetes and the patient’s insulin resistance, the OBGYN believes that metformin will be the best first step toward managing this condition. The doctor says that if regular periods don’t return to consider other steps such as birth control. The patient has concerns about taking medication because she has never been on any long-term medication. The doctor says that the only possible alternative would be to make lifestyle changes to diet and exercise so that she can lower her glucose levels and insulin levels. When prescribing the metformin to patient A, the provider tells her that a slow ingestion of metformin will be the best way. This is because metformin is known to cause gastrointestinal issues. The doctor’s ultimate goal is for patient A to take 1000mg twice a day, evening and night. The slow uptake of metformin is necessary to mitigate the side effects of metformin.
As of right now, Patient A is currently managing her Polycystic Cystic Ovarian Syndrome through annual doctors’ visits with her OBGYN and her primary care provider. Despite some of the Gastrointestinal issues, she is taking metformin at a lower dosage. It has been effective in making her periods regular and lowering the insulin resistance she was experiencing. She is also currently working on losing weight by making lifestyle changes to her diet and exercise. Overall, case study A allows us to get an overview of the reasons why the OBGYN was able to correctly diagnose and ultimately treat patient A. This hopefully can aid providers in being able to effectively diagnose patients by recognizing the possible signs of PCOS; As well as help the general public be aware of some possible symptoms of PCOS that may apply to their current health condition, so they can advocate for the correct treatment for themselves.
- Kyrou, I., Weickert, M. O., & Randeva, H. S. (2015). Diagnosis and Management of Polycystic Ovary Syndrome (PCOS). In R. Ajjan & S. M. Orme (Eds.), Endocrinology and Diabetes: Case Studies, Questions and Commentaries (pp. 99–113). Springer. https://doi.org/10.1007/978-1-4471-2789-5_13. ↵
- Calvo, F., Karras, B. T., Phillips, R., Kimball, A. M., & Wolf, F. (2003). Diagnoses, Syndromes, and Diseases: A Knowledge Representation Problem. AMIA Annual Symposium Proceedings, 2003, 802. ↵
- Joo, Y. Y., Actkins, K., Pacheco, J. A., Basile, A. O., Carroll, R., Crosslin, D. R., Day, F., Denny, J. C., Velez Edwards, D. R., Hakonarson, H., Harley, J. B., Hebbring, S. J., Ho, K., Jarvik, G. P., Jones, M., Karaderi, T., Mentch, F. D., Meun, C., Namjou, B., … Hayes, M. G. (2020). A Polygenic and Phenotypic Risk Prediction for Polycystic Ovary Syndrome Evaluated by Phenome-Wide Association Studies. The Journal of Clinical Endocrinology and Metabolism, 105(6), 1918–1936. https://doi.org/10.1210/clinem/dgz326. ↵
- Acanthosis Nigricans—American Osteopathic College of Dermatology (AOCD). (n.d.). Retrieved October 16, 2023, from https://www.aocd.org/page/AcanthosisNigricans. ↵
- Rawla, M. F. B. P. (2019). English: Acanthosis nigricans on axilla. https://www.ncbi.nlm.nih.gov/books/NBK431057/. https://commons.wikimedia.org/wiki/File:Acanthosis_nigricans.jpg ↵
- Christ, J. P., & Cedars, M. I. (2023a). Current Guidelines for Diagnosing PCOS. Diagnostics, 13(6), 1113. https://doi.org/10.3390/diagnostics13061113. ↵
- Dandelion Medical Animation (Director). (2023, January 14). Menstruation and Polycystic Ovary Syndrome or PCOS | Causes |Treatments|Dandelion Medical Animation. https://www.youtube.com/watch?v=Mc5iK0AtGNc. ↵
- Progesterone: Natural Function, Levels & Side Effects. (n.d.). Cleveland Clinic. Retrieved October 20, 2023, from https://my.clevelandclinic.org/health/body/24562-progesterone ↵
- Dandelion Medical Animation (Director). (2023, January 14). Menstruation and Polycystic Ovary Syndrome or PCOS | Causes |Treatments|Dandelion Medical Animation. https://www.youtube.com/watch?v=Mc5iK0AtGNc. ↵
- Christ, J. P., & Cedars, M. I. (2023a). Current Guidelines for Diagnosing PCOS. Diagnostics, 13(6), 1113. https://doi.org/10.3390/diagnostics13061113. ↵
- Iatrakis, G., Tsionis, C., Adonakis, G., Stoikidou, M., Anthouli-Anagnostopoulou, F., Parava, M., Vouxinou, A., Georgopoulos, N. A., & Kourounis, G. (2006). Polycystic ovarian syndrome, insulin resistance and thickness of the endometrium. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 127(2), 218–221. https://doi.org/10.1016/j.ejogrb.2006.01.023. ↵
- Androgens: Function, Measurement and Related Disorders. (n.d.). Cleveland Clinic. Retrieved October 20, 2023, from https://my.clevelandclinic.org/health/articles/22002-androgens. ↵
- Christ, J. P., & Cedars, M. I. (2023a). Current Guidelines for Diagnosing PCOS. Diagnostics, 13(6), 1113. https://doi.org/10.3390/diagnostics13061113. ↵
- DHEAS Test: What It Is, Procedure, Results. (n.d.). Cleveland Clinic. Retrieved October 20, 2023, from https://my.clevelandclinic.org/health/diagnostics/22148-dheas-test-dhea-sulfate-test. ↵
- Nonalcoholic Fatty Liver Disease. (2019, November 19). https://www.hopkinsmedicine.org/health/conditions-and-diseases/nonalcoholic-fatty-liver-disease. ↵
- Gnawali, A., Patel, V., Cuello-Ramírez, A., Al kaabi, A. S., Noor, A., Rashid, M. Y., Henin, S., & Mostafa, J. A. (n.d.). Why are Women With Polycystic Ovary Syndrome at Increased Risk of Depression? Exploring the Etiological Maze. Cureus, 13(2), e13489. https://doi.org/10.7759/cureus.13489. ↵
- Metformin in obesity, cancer, and aging: Addressing controversies—PMC. (n.d.). Retrieved October 20, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384433/. ↵
- Metformin in obesity, cancer and aging: Addressing controversies—PMC. (n.d.). Retrieved October 20, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384433/. ↵
- Nasri, H., & Rafieian-Kopaei, M. (2014). Metformin: Current knowledge. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 19(7), 658–664. ↵
- Mayo Clinic Explains Insulin Resistance—YouTube. (n.d.). Retrieved October 20, 2023, from https://www.youtube.com/watch?v=vGjOxWweQ0g. ↵
- EVALUATION OF METFORMIN HYDROCHLORIDE DIRECT COMPRESSIBLE TABLET USING BY HICEL TM MICROCRYSTALLINE CELLULOSE EXCIPIENT. World Journal of Pharmaceutical Research, 5. https://doi.org/10.20959/wjpr201611-7364 ↵
- MedLecturesMadeEasy (Director). (2023, May 30). Polycystic ovarian syndrome, PCOS (mechanism of disease). https://www.youtube.com/watch?v=QWfigWOBmR0. ↵



2 comments
Muskaan Tayal
This essay is very informative and I learned a lot about PCOS. I also loved the images that you used. Amazing job Kelsey!
Mia Alexandra Gonzalez
I love this article, it goes over a lot if information I did not know about PCOS! Great job Kelsey!!!