It’s every woman’s nightmare, yet 1 in 8 women are destined to develop breast cancer in their lifetime. Most cases of breast cancer are developed through somatic mutations accumulated throughout a person’s lifetime; this means that it cannot be passed down to offspring. There is a smaller percentage of women who have an inherited cancer risk by obtaining mutations on the BRCA1 and BRCA2 genes from a parent.1
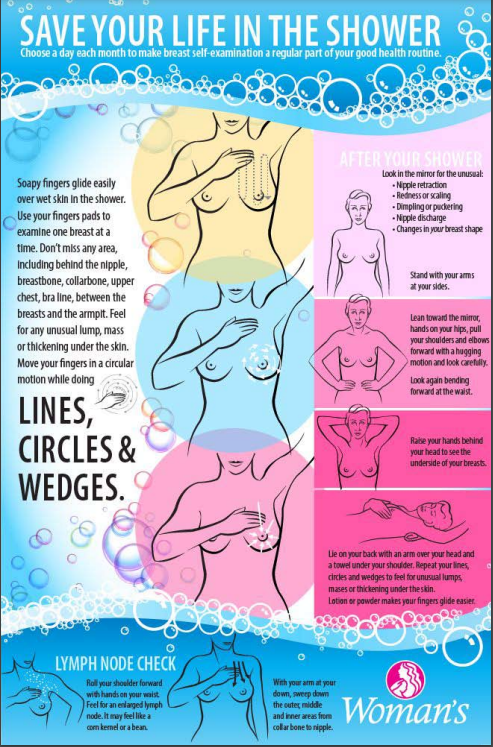
Alice, a 35-year-old mother of four children runs a busy life; she’s a secretary at her day job, takes her children to all their extracurricular activities, cooks dinner for the family, and keeps up with all the household chores. Lately, she has been feeling extra tired and thought nothing of it until one night while taking a shower, she noticed something was off. While doing a breast self-examination she felt a small lump, almost pea-sized underneath her skin. She set up an appointment with her gynecologist, where they did another clinical breast examination. Her doctor asked what other symptoms she had been experiencing, and Alice explained she also had bloody nipple discharge. Other symptoms found in breast cancer include inversion of the nipple, asymmetrical breast, breast skin thickening, and breast skin erythema (skin redness). Her doctor took a sample of the discharge to send out for testing on a slide and also did an in-clinic mammogram. A mammogram is an X-ray picture of the breast taken by having the woman stand in front of a special X-ray machine. A technologist will place your breast on a plastic plate, and another plate will come from above to press your breast. The plates will flatten your breasts and another angle, the side profile, will be done to image both breasts. A mammogram is usually uncomfortable for most women. Factors that play a role in discomfort include going the week before or on your menstrual cycle, the size of your breast, how much your breast needs to be pressed, and the skill of your technologist. It is usually recommended not to wear deodorant, perfume, or powder because these products can show up as white spots on the x-ray.
A couple of weeks went by before Alice was called into her gynecologist’s office with the results from the mammogram. It has been confirmed that the lump she found shows on the mammogram as a 2.0 cm mass. The next step for the doctor is to perform a biopsy, a definitive test for malignancy. A core needle biopsy allows microscopic examination of affected breast tissue and is done by inserting a hollow tube into an incision in the breast that is guided to the mass by an MRI, X-ray, or ultrasound. The affected breast tissue is then pulled into the tube with the help of a small spinning knife that is inside the tube. The sample will then be sent off to a pathologist to analyze the breast tissue. The TNM Classification of Malignant Tumors system, which is used to stage breast cancer and guide treatment, stands for tumor size (T), lymph nodes (N), and metastasis (M).2 The pathologist will also classify the stage of breast cancer, which ranges from 0, 1, 2, 3, and 4. Tumor size refers to the size and extent of the primary tumor; lymph nodes refer to the number of affected nodes and location of nodes with cancer; and metastasis refers to whether cancer has spread from the primary tumor location to other parts of the body. There are three steps involved in the process of metastasis. First, cancer cells invade surrounding tissues and vessels. The cells must detach for them to become invasive. Next, cancer cells are transported by the circulatory system to distant sites. Invading cells secrete proteases that degrade the extracellular matrix and basal lamina, which are usually barriers to cancer cell movement. Finally, cancer cells reinvade and grow at a new location. These cells must become motile in order to move from one place to another. Based on these characteristics of the TNM classification, the stage of breast cancer is determined. Stage 0 usually refers to precancer or carcinoma in situ; abnormal cells that look like cancer are found in the place they originally formed and have not spread to other nearby tissues. Stage 4 is referred to as metastatic breast cancer.
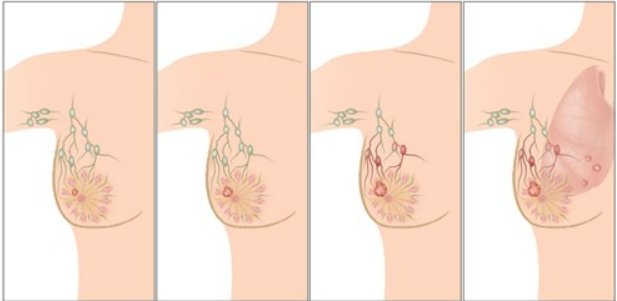
Cancer is not only found in the breast and nearby lymph nodes but has also traveled to other organs as well. It can also mean that recurrence of breast cancer has spread to other areas. Common sites of metastases for breast cancer include: lungs, skin, bones, liver, brain and distant lymph nodes. Tumor grade will also be determined which ranges from 1-3. This is an examination of the cancer cells to determine how (aggressive) fast or slow they are growing. Alice’s doctor sets another appointment, she needs to check if her breast cancer has spread. According to Jafari, an MRI is an important diagnostic tool for breast cancer. MRI’s can be used in monitoring response to therapy, assessing metastasis of breast cancer and checking if a tumor has returned.3,4 An MRI uses contrast agents which are able to improve the sensibility of images in the region of interest. Other diagnostic tools include multiple different types of scans that can determine if cancer has spread. PET scans use radioactive isotopes, which emit positrons. Ultrasounds use sound waves to produce images of body parts that are getting scanned. CT scans can take as little as 10 minutes or more depending on what part of the body is getting scanned. Another factor to consider with CT scans is if IV contrast is being used, it may take longer to obtain the scan. Chest X-rays will also be used to see if breast cancer has metastasized in the lungs.
It’s time to reveal her results to her, based on size and all other factors taken into consideration. The doctor has determined that Alice has Stage 2B breast cancer due to the size of her tumor and the fact that it may have potentially spread to axillary lymph nodes. There is one more thing to check, and that is if this cancer is responsive to hormones. The way to check would be genetic testing. It is called a BRCA gene test and is done by collecting blood, saliva, or cells inside the cheek. The sample is then sent to a lab for DNA analysis.
About 5-10 percent of women who develop breast cancer have inherited mutations that predispose them. A mutation in the BRCA1 gene will cause carriers to have a significantly increased chance of developing breast or ovarian cancer. A mutation in the gene causes the development of cancer by promoting growth factors in breast tissue.5
Alice waits patiently, but these results usually take weeks or even months. After a little over a month, Alice receives her results, she is BRCA1 positive. What does this mean? What does this gene do? The BRCA1 gene is expressed in multiple tissues, such as breast and ovarian tissue.1 It is composed of 22 exons which encode a 220 kDa nuclear protein of 1863 amino acids. BRCA1 and BRCA2 genes function as tumor suppressor genes, they code for proteins involved in DNA damage and keep the cell cycle functioning optimally. BRCA genes aid in pathways that recognize and correct double-stranded breaks of certain DNA damages. These mutations are usually point mutations or deletion/insertion mutations. In reaction to these mutations, p53-dependent DNA breakdown is activated, which leads to cell cycle arrest and apoptosis.7 A positive test result means that Alice has inherited a known harmful variant of BRCA1, most likely from her mother. Testing, such as mammograms, for family members should be carried out 10 years before the affected family member was diagnosed with cancer.
It is finally time to talk about treatment for her breast cancer. Alice will meet with an oncologist who has collected all her scans including mammograms, ultrasounds, and a CT, blood work, and genetic testing results, in order to formulate a treatment plan for her. There are multiple different surgeries that are used to treat breast cancer, but factors that play a role are the size and metastasis into lymph nodes or surrounding tissue. Surgical removal of the tumor is usually the first step in the treatment for breast cancer. Usually, for tumors that have not invaded surrounding lymph nodes, a lumpectomy is recommended, where they simply excise the tumor. However, what Alice will need since her cancer has spread to surrounding lymph nodes is something called a mastectomy. A lumpectomy would be considered too risky, possibly leaving some cancer cells that can later metastasize.5 Regardless of her current choice and because of her young age, Alice may choose to have a double mastectomy to prevent the chances of getting recurring breast cancer. Even opting to have a complete hysterectomy may diminish the chances of having breast cancer once again or even developing ovarian cancer. The lowered risk of developing breast cancer comes from the removal of the ovaries. The ovaries produce female hormones such as estrogen and progesterone, and breast cancer is known to grow in response to excess estrogen.
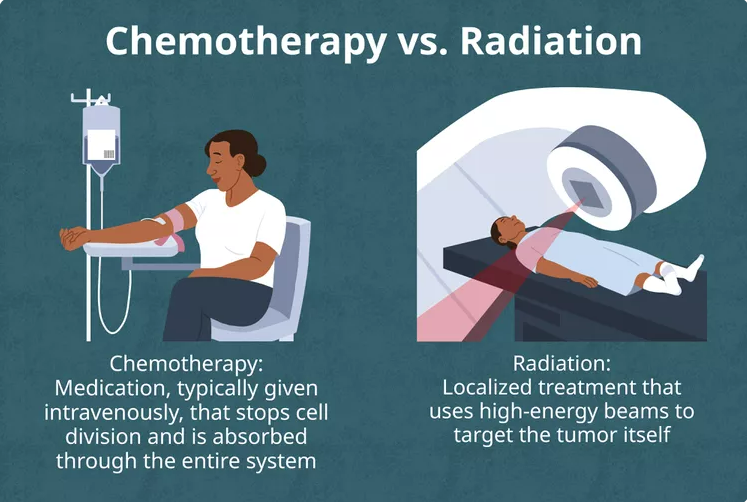
After Alice’s surgery, in which she opted for a mastectomy and lymph node removal, it will take her approximately 3-6 weeks to fully recover after a one-night stay at the hospital. But the fight is not over yet her oncologist has determined she will need both chemotherapy and radiation in addition to the surgery. Surgical treatment has evolved in the past couple of decades, advances aim to minimize the amount of therapy needed to cure cancer. However, sometimes other therapies are needed in addition to surgery.9 Alice is set to receive her first round of chemotherapy, Doxorubicin (“red devil”), just two weeks after her mastectomy and will receive three more rounds every three weeks after that. Next, she will have 25 rounds of radiation every day after getting marked with small tattoos as markers. The beam of intense energy X-rays damages cancerous cells by destroying their genetic material. Finally, she opts to have a complete hysterectomy to decrease her chances of recurring breast or ovarian cancers. After 2 years, Alice’s breast cancer is in remission, and she is now considered a breast cancer survivor. Annual checks with her gynecologist and oncologist for screenings will help make sure that she can stay healthy and in remission. Mammograms use radiation which causes double-stranded breaks in DNA, which in turn affects the BRCA1 gene because of its responsibility of repairing DNA double-strand break repair through homologous recombination. Her doctors have determined that the benefit of finding cancer fast through annual mammograms outweighs the risks of gaining mutations through x-ray exposure due to mammograms. Starting at age 40, women are recommended to start getting annual mammograms to screen for cancer. Her young daughters will now have to look out for their health and start standard screenings at a much younger age than is normally recommended.
- Godet, I., & Gilkes, D. M. (2017). BRCA1 and BRCA2 mutations and treatment strategies for breast cancer. Integrative Cancer Science and Therapeutics, 4(1), 10.15761/ICST.1000228. ↵
- Teichgraeber, D. C., Guirguis, M. S., & Whitman, G. J. (2021). Breast Cancer Staging: Updates in the AJCC Cancer Staging Manual, 8th Edition, and Current Challenges for Radiologists, From the AJR Special Series on Cancer Staging. American Journal of Roentgenology, 217(2), 278–290. https://doi.org/10.2214/AJR.20.25223. ↵
- Jafari, S. H., Saadatpour, Z., Salmaninejad, A., Momeni, F., Mokhtari, M., Nahand, J. S., Rahmati, M., Mirzaei, H., & Kianmehr, M. (2018). Breast cancer diagnosis: Imaging techniques and biochemical markers. Journal of Cellular Physiology, 233(7), 5200–5213. https://doi.org/10.1002/jcp.26379. ↵
- Mann, R. M., Kuhl, C. K., Kinkel, K., & Boetes, C. (2008). Breast MRI: guidelines from the European Society of Breast Imaging. European radiology, 18, 1307-1318. ↵
- Crawford, Sarah, & Alder, Richard (2022). Magill’s Medical Guide (Online Edition), 2022, Research Starters,6. ↵
- Godet, I., & Gilkes, D. M. (2017). BRCA1 and BRCA2 mutations and treatment strategies for breast cancer. Integrative Cancer Science and Therapeutics, 4(1), 10.15761/ICST.1000228. ↵
- Varol, U., Kucukzeybek, Y., Alacacioglu, A., Somali, I., Altun, Z., & Tarhan, M. O. (2018). BRCA genes: BRCA 1 and BRCA 2. JBUON 23(4),863. ↵
- Crawford, Sarah, & Alder, Richard (2022). Magill’s Medical Guide (Online Edition), 2022, Research Starters,6. ↵
- Waks, A. G., & Winer, E. P. (2019). Breast Cancer Treatment: A Review. JAMA, 321(3), 288–300. https://doi.org/10.1001/jama.2018.19323. ↵



4 comments
jvillarreal68
Hi Gabriela! This was a very informative article about breast cancer and different ways to check and see the signs before the symptoms get serious. As a female, I feel like this is something every girl should be educated about since this is a very serious cancer. I personally had very little knowledge about breast cancer until a family member was diagnosed, but after reading your essay, I feel like I now know a lot more about it.
Johana Solís
Hi Gabriela! You’re article is very well informative. Loved the way you provided ways to check if anything is wrong with a women’s body. Something so scary can happen to any female and it is very important to hear and understand our bodies. Thank you for providing a short story about Alice it really helped understand what to do in case we notice something wrong.
Anapatricia Macias Angulo
Hi Gabriela! This is an excellent article- I love the way you included an example of a person to tell the story. You also made explanations of topics, like treatments and the different stages of breast cancer, simple to understand for the audience, especially for those who might not know much to begin with. Knowing how to conduct a self-exam is extremely important, and I like how you included a visual of how to do this. Thank you for sharing more information about a topic that touches and affects so many people around the world- wonderful job!
Esteban Serrano
Hi Gabriella. This article is very informative and compelling. The topic is one of great trauma because I know a few people who have lost their lives to forms of cancer, but especially breast. Your article put it into perspective with the story about the mother who noticed just the tiniest difference in anatomy, which basically prevented any growth. I am hoping, with the advanced technology and science knowledge we have now, that cancers of all forms can be treated and disappeared. Thank you for sharing!