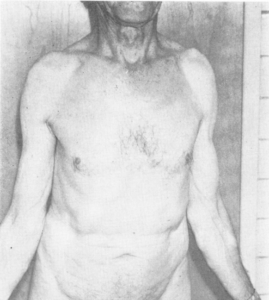
Dercum’s disease is a rare disorder consisting of multiple, painful lipomas subcutaneously distributed primarily in the trunk and the extremities. This disease was first described by an American neurologist, Dr. Dercum, in 1888. It was further demonstrated by Dr. White in 1899.1 There are reports in the literature that suggest that this disease may be an autoimmune disorder. Disturbances in endocrine function and improper breakdown (metabolism of fat have also been proposed as potentially playing a role in the development of the disorder). Synonyms for this disease found in the literature include adiposalgia, lipomatosis dolorosa, adipose tissue rheumatism, Ander syndrome, and morbus dercum. This disease is most commonly seen in women between 35-50 years of age. The symptoms most demonstrated in patients with Dercum’s disease include easy bruisability, sleep disturbances, impaired memory, depression, difficulty concentrating, anxiety, diabetes, fatigue, weakness, and joint aches.2 While the etiology is unclear,there are several theories that have been proposed, but none demonstrate clear evidence. Endocrine and nervous system dysfunction have been suspected but it had not been proven to be a factual aspect of the disease. Stretching and pressure on nerves from growing fatty masses has been suggested but does not show histopathologically.3 Inflammation is demonstrated to vary on histopathology between biopsies of lipomas of painful and non-painful areas in patients with Dercum’s disease.4,5
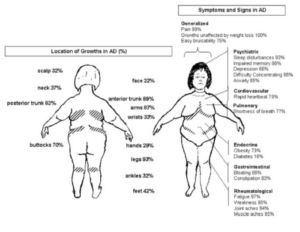
Dercum’s disease has been suggested to be classified into 4 distinct variants: type I has a generalized diffuse form presenting with diffusely widespread painful adipose tissue without clear lipomas; type II generalized nodular form presenting with widespread, painful adipose tissue with intense pain in and around multiple lipomas; type III- localized nodular form presenting with pain strictly surrounding lipomas; type IV the juxta- articular form presents as painful adipose tissue near large joints.7
The diagnostic criteria for Dercum’s disease include: 1) generalized overweight or obesity and 2) chronic pain (greater than 3 months) in the adipose tissue. A thorough exclusion of differential diagnosis is also necessary. There are no distinctive laboratory markers for the disease. The pathohistological picture biopsies of fat tissue are generally indistinguishable from lipomas. An MRI scan may show multiple small, oblong, fatty lesions in subcutaneous tissue. An ultrasound may show hyper-echoic nodules.8

Differential diagnoses that should be considered include fibromyalgia, panniculitis, endocrine disorders such as Cushing’s disease and hypothyroidism, Madelung syndrome, familial multiple lipomatosis, and proteus syndrome. Fibromyalgia is a common chronic syndrome of widespread musculoskeletal pain and tenderness, fatigue, and cognitive difficulties that can be easily confused is adiposis dolorosa, especially in overweight or obese females. These patients also have unremarkable physical examinations and lab work. The diagnosis is also based on widespread pain and tender points that are typically in specific locations in muscles and joints. Panniculitis presents as painful, inflammatory masses of subcutaneous fat. This is characterized by tender skin nodules and systemic signs. The diagnosis is made with a skin biopsy to determine the septal or lobular features and the presence of types of subcutaneous inflammatory infiltrates. Endocrine disorders that are often confused with Dercum’s Disease include Cushing’s syndrome and hypothyroidism. Both of these conditions present with weight gain and generalized pain that is not localized to subcutaneous tissue. Madelung syndrome also known as Launois Bensaude syndrome, is a form of multiple symmetric lipomatosis that is primarily located in the upper body (shoulders, neck, head) and is most commonly seen in men with chronic excessive alcohol consumption. Multiple deletions of mitochondrial DNA, MERRF, LIPE, and MNF2 mutations have been identified in nonalcoholic cases. Familial multiple lipomatosis corresponds to the occurrence of painless lipomas located in the arms and legs during adolescence. This is genetic with autosomal dominant inheritance, this has a mutation in the 12q13-15 region which contains the HMGA2 gene and PALB2 gene mutation. Proteus syndrome is a rare disorder characterized by disproportionate, asymmetric overgrowth of skin, bones, blood vessels, and fatty and connective tissue. This is caused by an activating mutation in the AKT1 oncogene.12
Treatment for Dercum’s disease primarily targets pain management. There is no current standard for treatment, but there are several treatment options described in several case reports for reducing symptoms. Unfortunately, lifestyle changes such as diet and exercise have not been proven to reduce fatty tissue. Surgical interventions such as liposuction and lipectomy do help to reduce pain, but this effect is not long-lasting. The mechanism of how these treatment options reduce pain is currently unknown. Lidocaine injection directly into lipomas demonstrates improvement in pain for up to 4 months. Lidocaine administered intravenously has shown improvement in pain for up to nine months. There are many medications have resulted in improvement in pain. NSAIDs were initially thought to be ineffective, but a study by Herbst et al. demonstrates an 89% reduction in pain for patients with Dercum’s disease. There are also case reports that support the potential of pregabalin13, D-amphetamine14, metformin15, interferon a-2b16, infliximab and methotrexate17 in pain management. There are also some noninvasive procedures that have been described as beneficial. Treatment with a transcutaneous frequency rhythmic electrical modulation system for over a period of six months is noted to improve pain and reduce fat tissue in a patient with Dercum’s disease.18 Four weeks of deep tissue massage has demonstrated a significant decrease in weight, but no change in pain has been reported.19
There are support groups available including Dercum Society20, Oregon Lipedema/Dercum Disease Support Group21, and the Australia Dercum’s Disease Support Group22
Management of this disease has been proven to be difficult since there is no standard of care for symptom control.
- White, H. (1899). A Case of Adiposis Dolorosa.British Medical Journal,2(2031), 1533-1534.1. ↵
- Hansson, E., Svensson, H., & Brorson, H. (2012). Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet Journal of Rare Diseases, 7(1), 23. https://doi.org/10.1186/1750-1172-7-23. ↵
- Hansson, E., Svensson, H., & Brorson, H. (2012). Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet Journal of Rare Diseases, 7(1), 23. https://doi.org/10.1186/1750-1172-7-23. ↵
- Wollina, U., Heinig, B., Langner, D., & Nowak, A. (2015). Juxta-articular adiposis dolorosa (Dercum’s disease type IV.): Report of four cases and treatment by dermolipectomy. Wiener Medizinische Wochenschrift (1946), 165(17–18), 374–377. https://doi.org/10.1007/s10354-015-0378-1. ↵
- Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet Journal of Rare Diseases, 7, 23. https://doi.org/10.1186/1750-1172-7-23. ↵
- Herbst, K. L., & Asare-Bediako, S. (2007). Adiposis Dolorosa Is More Than Painful Fat. The Endocrinologist, 17(6), 326. https://doi.org/10.1097/TEN.0b013e31815942294. ↵
- Moattari, C., Giovane, R. A., & DiGiovanni Kinsely, S. (2020). Dercum’s disease: A Case Report of a Patient Having Both Type 1 and Type 2 Dercum’s Disease. Case Reports in Dermatological Medicine, 2020, 6129706. https://doi.org/10.1155/2020/6129706. ↵
- Hansson, E., Svensson, H., & Brorson, H. (2012). Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet. ↵
- Lynch, H. T., & Harlan, W. L. (1963). Hereditary Factors in Adiposis Dolorosa (Dercum’s disease). American Journal of Human Genetics, 15(2), 184–190. ↵
- Moattari, C., Giovane, R. A., & DiGiovanni Kinsely, S. (2020). Dercum’s disease: A Case Report of a Patient Having Both Type 1 and Type 2 Dercum’s Disease. Case Reports in Dermatological Medicine, 2020, 6129706. https://doi.org/10.1155/2020/6129706. ↵
- Crescenzi, R., Donahue, P. M. C., Weakley, S., Garza, M., Donahue, M. J., & Herbst, K. L. (2019). Lipedema and Dercum’s disease: A New Application of Bioimpedance. Lymphatic Research and Biology, 17(6), 671–679. https://doi.org/10.1089/lrb.2019.0011. ↵
- Cook, J. C., & Gross, G. P. (2023). Adiposis Dolorosa. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK507867/. ↵
- Ghazala, S., Bilal, J., Ross, E., Riaz, I. B., Kalb, B., & Herbst, K. L. (2018). Low-Dose d Amphetamine Induced Regression of Liver Fat Deposits in Dercum Disease. The America Journal of Medicine, 131(6), 705–708. https://doi.org/1016/j.amjmed.2017.12.026 ↵
- Ghazala, S., Bilal, J., Ross, E., Riaz, I. B., Kalb, B., & Herbst, K. L. (2018). Low-Dose d Amphetamine Induced Regression of Liver Fat Deposits in Dercum Disease. The America Journal of Medicine, 131(6), 705–708. https://doi.org/10.1016/j.amjmed.2017.12.026. ↵
- Łabuzek, K., Liber, S., Suchy, D., & Okopień, B. (2013). A successful case of pain management using metformin in a patient with adiposis dolorosa. International Journal of Clinical Pharmacology and Therapeutics, 51(6), 517–524. https://doi.org/10.5414/cp201878. ↵
- Gonciarz, Z., Mazur, W., Hartleb, J., Machniak, M., Bednarek, I., Mazurek, U., & Wilczok, T. (1997). Interferon alfa-2b induced long-term relief of pain in two patients with adiposis dolorosa and chronic hepatitis C. Journal of Hepatology, 27(6), 1141. https://doi.org/10.1016/S0168-8278(97)80164-X. ↵
- Meiss, F., Helmbold, P., Meykadeh, N., Gaber, G., Marsch, Wc., & Fischer, M. (2007). Overlap of acute generalized exanthematous pustulosis and toxic epidermal necrolysis: Response to antitumour necrosis factor‐α antibody infliximab: report of three cases. Journal of the European Academy of Dermatology and Venereology, 21(5), 717–719. https://doi.org/10.1111/j.1468-3083.2006.02026.x. ↵
- Martinenghi, S., Caretto, A., Losio, C., Scavini, M., & Bosi, E. (2015). Successful Treatment of Dercum’s disease by Transcutaneous Electrical Stimulation. Medicine, 94(24), e950. https://doi.org/10.1097/MD.0000000000000950. ↵
- Ibarra, M., Eekema, A., Ussery, C., Neuhardt, D., Garby, K., & Herbst, K. L. (2018). Subcutaneous adipose tissue therapy reduces fat by dual X-ray absorptiometry scan and improves tissue structure by ultrasound in women with lipoedema and Dercum disease. Clinical Obesity, 8(6), 398–406. https://doi.org/10.1111/cob.12281. ↵
- The Dercum Society• Helping make sense of Dercum’s Disease. (n.d.). Retrieved November 1, 2023, from https://dercums.org/. ↵
- Home | Oregon Lipedema/Dercum Disease Support Group. (n.d.). OLDDSG. Retrieved November 1, 2023, from https://www.oregonlddsg.com. ↵
- The Australia Dercum’s Disease Support Group – Rare Voices Australia. (n.d.). Retrieved November 1, 2023, from https://rarevoices.org.au/rva-support-organisa/australia-dercums-disease-support-group/. ↵


1 comment
Dylan Vargas
I have never heard about Dercum’s disease before reading this article. I love how the author explains the different syndromes and ages the symptoms show up like how it is most related to women between 35-50 years of age. Even how there are different variants which I had no idea about. Being able to explain all the different ways this disease works and why it exists is very interesting. Though looks like there is no cure and even going on a diet doesn’t even work, which is unfortunate. Though this article is well done and very informative.